
Wilmington (937) 382-2347
Fax
(513) 932-1606

Wilmington (937) 382-2347
Fax
(513) 932-1606
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.

Cracked heels, a common foot condition, often arise from dry skin, which can be exacerbated by various medical conditions. For instance, individuals with diabetes may develop neuropathy, a nerve condition that impairs the ability to sweat, leading to increased skin dryness. This lack of perspiration contributes significantly to the development of dry, cracked heels. Similarly, Sjogren’s syndrome, predominantly observed in women, is an autoimmune disorder where the body mistakenly attacks its moisture-producing glands, including those responsible for perspiration. This attack results in notably dry skin, heightening the risk of cracked heels. Additionally, specific skin conditions such as psoriasis, eczema, and fungal infections directly affect the skin's moisture balance. These conditions lead to the skin becoming dry and less elastic, making it more prone to cracking, especially in the heel area, which bears significant weight and pressure during walking and standing. These medical factors underscore the importance of understanding and managing underlying health conditions to prevent or treat cracked heels effectively. If you have cracked heels, it is suggested that you schedule an appointment with a podiatrist for an evaluation and a determination of whether there is an underlying medical problem, in addition to receiving correct treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Dr. Gerald Perelman from Ohio. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Wilmington, OH . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
 A podiatrist, known as a foot and ankle specialist, is a healthcare professional dedicated to the diagnosis, treatment, and prevention of conditions affecting the lower extremities. With an emphasis on maintaining optimal foot health, podiatrists address a diverse array of issues, including but not limited to, bunions, ingrown toenails, and biomechanical abnormalities. Becoming a podiatrist involves a rigorous educational journey. Aspiring professionals typically embark on a Doctor of Podiatric Medicine, or DPM program, which encompasses comprehensive studies in anatomy, physiology, and clinical rotations focusing on podiatric medicine and surgery. This extensive education equips podiatrists with the knowledge and skills necessary to provide specialized care for foot and ankle ailments. The dedication to this unique branch of healthcare ensures that podiatrists are well-versed in the complexities of lower limb conditions. If you have foot or ankle problems or are interested in pursuing podiatry as a career choice, it is suggested that you confer with this type of doctor who can provide care and information sought.
A podiatrist, known as a foot and ankle specialist, is a healthcare professional dedicated to the diagnosis, treatment, and prevention of conditions affecting the lower extremities. With an emphasis on maintaining optimal foot health, podiatrists address a diverse array of issues, including but not limited to, bunions, ingrown toenails, and biomechanical abnormalities. Becoming a podiatrist involves a rigorous educational journey. Aspiring professionals typically embark on a Doctor of Podiatric Medicine, or DPM program, which encompasses comprehensive studies in anatomy, physiology, and clinical rotations focusing on podiatric medicine and surgery. This extensive education equips podiatrists with the knowledge and skills necessary to provide specialized care for foot and ankle ailments. The dedication to this unique branch of healthcare ensures that podiatrists are well-versed in the complexities of lower limb conditions. If you have foot or ankle problems or are interested in pursuing podiatry as a career choice, it is suggested that you confer with this type of doctor who can provide care and information sought.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. Gerald Perelman from Ohio. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Wilmington, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
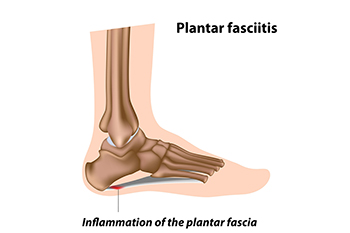
Plantar fasciitis, a commn cause of heel pain, is a condition that occurs when the plantar fascia, a thick band of tissue that connects the heel bone to the toes, becomes inflamed and irritated. Several common factors contribute to the development of plantar fasciitis. One primary cause is excessive or repetitive strain on the feet. This often results from activities that place a significant burden on the plantar fascia, like prolonged standing, walking, or running, especially on hard surfaces. Footwear with inadequate arch support or cushioning can exacerbate the condition. Sudden weight gain or obesity is another contributing factor, as it places additional pressure on the feet. Tight calf muscles and Achilles tendons can also lead to plantar fasciitis by altering the mechanics of the foot, affecting the way it absorbs shock and distributes weight. Understanding these common causes is essential for both preventing and managing plantar fasciitis. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can effectively diagnose and treat this condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Gerald Perelman from Ohio. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Wilmington, OH . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
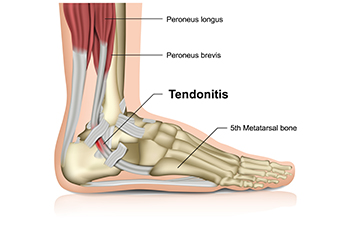
An Achilles tendon rupture is a severe and painful injury that affects the Achilles tendon, which is the largest and strongest tendon in the human body. Located at the back of the ankle, this vital band of connective tissue plays a pivotal role in facilitating walking, running, and jumping. When it tears, it can lead to excruciating pain, a loud popping sensation, and the inability to bear weight on the affected leg. The injury often occurs during sports or physical activities that involve sudden, forceful movements. An Achilles tendon rupture is more common among individuals aged 30 to 40, particularly men. It is beneficial to seek immediate medical attention from a podiatrist who can properly diagnose and treat this painful condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Gerald Perelman of Ohio. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Wilmington, OH . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.